Is it always possible to install a prosthesis?
Prosthetics is one of the most rapidly developing areas of medical technologies. Just 5-7 years ago, many of the solutions available today seemed like an absolute fantasy. Nowadays, creation of a high-quality prosthesis implies a strictly individual approach — there is no clear size guide or set of ready-made solutions. Top ranking prosthetic companies look at each case individually and make an informed decision about how best to help a particular person in a particular situation.
Therefore, it is impossible to answer the question of whether it is possible to install a prosthesis knowing only the diagnosis. Most likely, additional data will be required. It is important for you to understand that new technologies emerge every year. If a solution to the problem cannot be found right now, this does not mean that it will not be found after some time.
Therefore, it is impossible to answer the question of whether it is possible to install a prosthesis knowing only the diagnosis. Most likely, additional data will be required. It is important for you to understand that new technologies emerge every year. If a solution to the problem cannot be found right now, this does not mean that it will not be found after some time.
It is important for you to understand that new technologies emerge every year. If a solution to the problem cannot be found right now, this does not mean that it will not be found after some time.
Is it always possible to install a prosthesis?
It must be understood that, despite the unstoppable progress in the field of prosthetics, an “artificial” hand is not yet capable of replacing a real one. Why? Mainly, because of the limited number of possible movements and the lack of tactile sensitivity (that is, the prosthesis cannot feel the object you are touching). This is why you cannot equate a prosthesis with a hand. Then, why is prosthetics recommended by all international medical communities, regardless of whether there is a functional need for it or not?
To answer this question, it is necessary to understand what secondary health changes occur in people with upper limb disabilities. Secondary health problems imply changes that occur as a result of an underlying disease or disability. In our situation, this is an upper limb disability acquired at birth or as a result of injury/surgery.
To answer this question, it is necessary to understand what secondary health changes occur in people with upper limb disabilities.
Muscle hypotrophy of the arm requiring prosthetics.
The hand that requires prosthetics is not able to bear the required load. It is limited in its functions. This is called a “functional deficit.” Our patients often say that they try to actively use their hand in everyday activities even without a prosthesis. These are not the same thing — even if a person is used to using their hand as much as possible, they cannot take objects with it. However, holding objects and manipulating them is a necessary load for the limb muscles.
Posture disorders.
When the arm is shortened on one side, not only the functional deficit mentioned in the first paragraph is observed, but also a weight deficit. One side of the body weighs more than the other. Because of these two factors, the back muscles on one side are significantly weaker than on the other. At first, such disorders are noticeable at the muscle level only. However, muscles do not exist on their own; they are attached to bone structures and, if the muscles are developed asymmetrically, the changes eventually will affect the spine as well. A sideways spinal curvature is called scoliosis. Unlike an isolated muscle disorder, scoliosis is persistent and extremely difficult to correct. The back begins to hurt, and the severity of the pain may gradually increase. “Neglected” scoliosis can cause deformation of the viscera.
Second arm overload syndrome.
With a unilateral upper limb disability, the load between the two arms is distributed unevenly. Therefore, the joints, muscles, ligaments and fascia of a conditionally healthy hand are constantly overloaded. In foreign literature, this is called overuse syndrome — the second arm begins to hurt and requires close monitoring, and, most likely, treatment. Naturally, this develops not at once but with prolonged refusal of the prosthesis and overload of the healthy hand.
Thus, when the arm is shortened, the three secondary health changes mentioned above can be encountered most often. However, they are predictable and, therefore, preventable. The first thing we can do to prevent them is to regularly use an active prosthesis.
Why active and not cosmetic? An active prosthesis not only compensates for the weight difference between the two arms, but also puts a load on the muscles and joints, ensuring grasp and the ability to manipulate objects. From a medical point of view, active prosthess have a more pronounced positive effect on the body.
Thus, you may not equate a prosthesis with a hand, but you have to equate a prosthesis with health. Is it important to prevent secondary health problems? Definitely, yes. Can you do it without a prosthesis? Yes, but you will have to make a lot more effort.
To answer this question, it is necessary to understand what secondary health changes occur in people with upper limb disabilities. Secondary health problems imply changes that occur as a result of an underlying disease or disability. In our situation, this is an upper limb disability acquired at birth or as a result of injury/surgery.
To answer this question, it is necessary to understand what secondary health changes occur in people with upper limb disabilities.
Muscle hypotrophy of the arm requiring prosthetics.
The hand that requires prosthetics is not able to bear the required load. It is limited in its functions. This is called a “functional deficit.” Our patients often say that they try to actively use their hand in everyday activities even without a prosthesis. These are not the same thing — even if a person is used to using their hand as much as possible, they cannot take objects with it. However, holding objects and manipulating them is a necessary load for the limb muscles.
Posture disorders.
When the arm is shortened on one side, not only the functional deficit mentioned in the first paragraph is observed, but also a weight deficit. One side of the body weighs more than the other. Because of these two factors, the back muscles on one side are significantly weaker than on the other. At first, such disorders are noticeable at the muscle level only. However, muscles do not exist on their own; they are attached to bone structures and, if the muscles are developed asymmetrically, the changes eventually will affect the spine as well. A sideways spinal curvature is called scoliosis. Unlike an isolated muscle disorder, scoliosis is persistent and extremely difficult to correct. The back begins to hurt, and the severity of the pain may gradually increase. “Neglected” scoliosis can cause deformation of the viscera.
Second arm overload syndrome.
With a unilateral upper limb disability, the load between the two arms is distributed unevenly. Therefore, the joints, muscles, ligaments and fascia of a conditionally healthy hand are constantly overloaded. In foreign literature, this is called overuse syndrome — the second arm begins to hurt and requires close monitoring, and, most likely, treatment. Naturally, this develops not at once but with prolonged refusal of the prosthesis and overload of the healthy hand.
Thus, when the arm is shortened, the three secondary health changes mentioned above can be encountered most often. However, they are predictable and, therefore, preventable. The first thing we can do to prevent them is to regularly use an active prosthesis.
Why active and not cosmetic? An active prosthesis not only compensates for the weight difference between the two arms, but also puts a load on the muscles and joints, ensuring grasp and the ability to manipulate objects. From a medical point of view, active prosthess have a more pronounced positive effect on the body.
Thus, you may not equate a prosthesis with a hand, but you have to equate a prosthesis with health. Is it important to prevent secondary health problems? Definitely, yes. Can you do it without a prosthesis? Yes, but you will have to make a lot more effort.
How to choose the type of prosthesis?
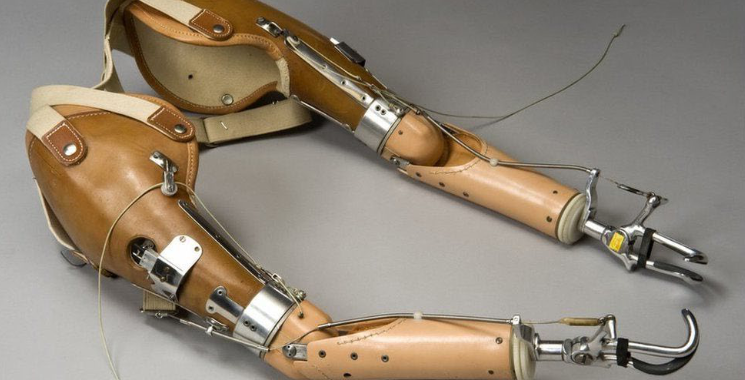
In the previous section, we used a number of terms (particularly names of prostheses), which may be unfamiliar to you. Let's take a step back and figure out what types of prostheses exist, and what their differences, advantages and disadvantages are.
Prostheses can be divided depending on the level of amputation or developmental challenges. For example, upper limb prostheses at the level of the hand and fingers, forearm prostheses, shoulder prosthesis and prostheses after shoulder disarticulation.
It is important to understand that this classification is not an absolute algorithm of actions. For example, if you have no fingers but a palm, this does not necessarily mean that you need a hand prosthesis. If the palm is immobile, that is, the wrist joint is malformed or restrained due to an injury, a hand prosthesis may not be suitable: you just would not be able to control it. Understanding all the details of this example is not important now, since each hand is individual. With this example we want to emphasize how important it is to approach the selection of a prosthesis carefully, and use the specialist knowledge in different fields.
Prostheses can be divided depending on the level of amputation or developmental challenges. For example, upper limb prostheses at the level of the hand and fingers, forearm prostheses, shoulder prosthesis and prostheses after shoulder disarticulation.
It is important to understand that this classification is not an absolute algorithm of actions. For example, if you have no fingers but a palm, this does not necessarily mean that you need a hand prosthesis. If the palm is immobile, that is, the wrist joint is malformed or restrained due to an injury, a hand prosthesis may not be suitable: you just would not be able to control it. Understanding all the details of this example is not important now, since each hand is individual. With this example we want to emphasize how important it is to approach the selection of a prosthesis carefully, and use the specialist knowledge in different fields.

Functional classification
Classification by the prosthesis capabilities is the most interesting and important for us. From a functional point of view, prostheses can be divided into three groups:
- Cosmetic
- Active
- Working
Prosthesis types in details
Cosmetic prostheses are intended to “mask” the absence of a limb or a part of it. They cannot restore the function of the hand. People often try to hold or press objects with such a prosthesis, but it is quite difficult to do this — the fingers of the prosthesis are not adapted for controlled movements, and do not obey their “master”. With modern prosthetics capabilities, we can match a cosmetic prosthesis that is close in skin color and even nail shape to the second hand; however, in our experience, it is impossible to achieve absolute identity, and the presence of the prosthesis is still noticeable.
Functional and cosmetic prostheses are capable of moving, or, more precisely, changing their position. This happens owing to external influence, for example, from a healthy hand. Roughly speaking, you can spread the fingers of the prosthesis, insert a spoon into them and fix them again. To be honest, such prosthetics are already quite obsolete, and you definitely would not see them on the streets of New York; that is why we do not produce them.
On the contrary, active prostheses involve active movements of the prosthesis fingers. Active movements are those, which are performed independently, that is, not by the other hand. These are exactly the kind of prostheses that our team produces.
Nonetheless, how does such a prosthesis understand what to do? When to flex and when to extend the fingers? These devices operate using various mechanisms. The first option is when the prosthesis has no external power source. The prosthesis moves owing to movements of the arm, on which it is installed. The simplest mechanism for such prostheses is a linkage mechanism. For example, the user bends the elbow or wrist, and at this time the links begin to move, flexing the prosthesis fingers. Such products are also called mechanical or pulling. The tutorial you are now reading has been created specifically for users of such prostheses.
Functional and cosmetic prostheses are capable of moving, or, more precisely, changing their position. This happens owing to external influence, for example, from a healthy hand. Roughly speaking, you can spread the fingers of the prosthesis, insert a spoon into them and fix them again. To be honest, such prosthetics are already quite obsolete, and you definitely would not see them on the streets of New York; that is why we do not produce them.
On the contrary, active prostheses involve active movements of the prosthesis fingers. Active movements are those, which are performed independently, that is, not by the other hand. These are exactly the kind of prostheses that our team produces.
Nonetheless, how does such a prosthesis understand what to do? When to flex and when to extend the fingers? These devices operate using various mechanisms. The first option is when the prosthesis has no external power source. The prosthesis moves owing to movements of the arm, on which it is installed. The simplest mechanism for such prostheses is a linkage mechanism. For example, the user bends the elbow or wrist, and at this time the links begin to move, flexing the prosthesis fingers. Such products are also called mechanical or pulling. The tutorial you are now reading has been created specifically for users of such prostheses.

The second option is a prosthesis with an external power source. In this case, the prosthesis has a motor that activates the device. The user has to give the correct command so that the prosthesis “knows” what action to perform. The most common method of “commanding” a prosthesis is bioelectric. User tenses a certain muscle, sensors inside the prosthesis read this tension and command the motor to “flex the fingers.” For the fingers to extend, you need to give a new command, for example, tense another muscle. Such prostheses are also called bioelectric or bionic.

Surely, bionic prostheses offer more opportunities and have more functions. They can hold heavier items. In addition, in some products the grasp can be adjusted differently — that is, fingers can be moved separately. However, it is important to understand that bionic prostheses are much more difficult to control. One muscle or another needs to be tensed while relaxing the others, and this is not an easy skill. Furthermore, because of the presence of additional elements, such prostheses are significantly heavier than active prostheses without an external power source.
It should be noted separately that in some cases installation of a bionic prosthesis is impossible, as the muscles are atrophied (have lost their strength due to forced inactivity), and the signal from them is insufficient to control the prosthesis. That is why opportune prosthetics are essential! We have prepared a dedicated tutorial on preparation for bionic prosthetics and the specifics of using a bionic prosthesis.
A separate chapter can be written about the appearance of Motorica active prostheses — because these products are created based on the user's design. The user chooses the color and pattern. In our opinion, it is important to avoid creating an analogue of the second hand. Trying to hide your differences is a path to low self-esteem rather than to acceptance of yourself and your body. Whatever the case, the choice is yours.
Finally, let’s discuss working prostheses. They require the availability of special attachments to perform certain functions. For example, for hammering or sewing. This is a separate broad area, which requires an in-depth individual approach.
It should be noted separately that in some cases installation of a bionic prosthesis is impossible, as the muscles are atrophied (have lost their strength due to forced inactivity), and the signal from them is insufficient to control the prosthesis. That is why opportune prosthetics are essential! We have prepared a dedicated tutorial on preparation for bionic prosthetics and the specifics of using a bionic prosthesis.
A separate chapter can be written about the appearance of Motorica active prostheses — because these products are created based on the user's design. The user chooses the color and pattern. In our opinion, it is important to avoid creating an analogue of the second hand. Trying to hide your differences is a path to low self-esteem rather than to acceptance of yourself and your body. Whatever the case, the choice is yours.
Finally, let’s discuss working prostheses. They require the availability of special attachments to perform certain functions. For example, for hammering or sewing. This is a separate broad area, which requires an in-depth individual approach.
Thus, globally, prostheses can be divided depending on the functions they perform — cosmetic (an attempt to create the appearance of having a hand) or active (movement and grasping).
The types of prostheses are summarized below in the following table:
The types of prostheses are summarized below in the following table:
How much does a prosthesis cost?
The cost of a prosthesis depends on its type and varies between different prosthetic companies.
It is important to understand that in accordance with current legislation Russian citizens regardless of age and region of residence, have the right to free provision of assistive devices and prosthetic and orthopedic appliances, which improve their level of independence in everyday life.
It is important to understand that in accordance with current legislation Russian citizens regardless of age and region of residence, have the right to free provision of assistive devices and prosthetic and orthopedic appliances, which improve their level of independence in everyday life.
When to install a prosthesis?
One of the general criteria for readiness to prosthetics in such cases is the integrity of the skin. There should be no wounds/abrasions/sutures on the skin. Immediately after amputation, the key role is played by caring for the stump, restoring sensitivity and functions of all the main body systems, and measures aimed at elimination of oedema (the standard option is elastic bandaging or special compression garments). All these factors are of high importance in deciding whether or not a prosthesis can be installed and when; so they should not be neglected.
Another fundamentally important condition for operation of the prosthesis without external power sources is the mobility of the superposed joint above the amputation. Superposed means preserved above the amputation site. For example, if the fingers are absent, it is the wrist joint; if the amputation is at the level of the forearm, it is the elbow joint, and so on. It is due to the flexion and extension of the joint that the prosthesis fingers move. Frequently, joint mobility in the early postoperative period is limited because of injury to surrounding tissues and swelling. Thus, the joint is fixed in a stationary position for a while. Therefore, after an injury or surgery, timely and comprehensive rehabilitation comes to the forefront to restore the previous mobility of the joint, create good muscle tone, and ensure the full functioning of the prosthesis.
Let’s consider particularly the cases of planned limb amputation. In these cases, we have time to prepare for the surgery and plan its scope in detail, taking into account future prosthetics. It is optimal to make decisions about the course of the upcoming surgery collectively — both by surgeons and prosthetists. This way, we can understand how best to shape the stump so that the prosthesis is easier to install and use.
Another fundamentally important condition for operation of the prosthesis without external power sources is the mobility of the superposed joint above the amputation. Superposed means preserved above the amputation site. For example, if the fingers are absent, it is the wrist joint; if the amputation is at the level of the forearm, it is the elbow joint, and so on. It is due to the flexion and extension of the joint that the prosthesis fingers move. Frequently, joint mobility in the early postoperative period is limited because of injury to surrounding tissues and swelling. Thus, the joint is fixed in a stationary position for a while. Therefore, after an injury or surgery, timely and comprehensive rehabilitation comes to the forefront to restore the previous mobility of the joint, create good muscle tone, and ensure the full functioning of the prosthesis.
Let’s consider particularly the cases of planned limb amputation. In these cases, we have time to prepare for the surgery and plan its scope in detail, taking into account future prosthetics. It is optimal to make decisions about the course of the upcoming surgery collectively — both by surgeons and prosthetists. This way, we can understand how best to shape the stump so that the prosthesis is easier to install and use.
Where can I get rehabilitation treatment after an injury or surgery?
The answer to this question depends largely on your residence and treatment location. Listing all the regional centers would take several dozen pages. However, even if there is no such a center near you or your experience of rehabilitation there makes you doubt the need for a repeat visit, remember about federal centers in large cities. Motorica can help you to get a referral for rehabilitation at them. In difficult cases — with combined injuries or lack of resources to visit federal centers — you can seek help from charity foundations. There is no shame in asking for help.
At what age would I fail to learn a prosthesis operation?
According to international recommendations, in case of lipomeria the first prosthesis should be installed at the age of six months. At this age, a cosmetic prosthesis is installed. Its main purpose is NOT to "disguise" a specific hand. After all, a child’s hand is beautiful in any case and there is absolutely no reason to hide it. The main goal of cosmetic prosthetics at this age is to compensate for the weight deficit and equalize the weight of both sides of the body.
Why is prosthetics recommended at six months? Because at about this age the child begins to sit up, and this is a task that requires a sense of equilibrium. “Catching” this equilibrium requires relatively equal weight of the hands.
Next, the baby masters new motor functions — crawls, stands up, begins to walk — and they also need an even load on both sides of the body. It is important to understand: the more part of the arm is missing, the greater the need for a cosmetic prosthesis from a very early age.
The transition to an active prosthesis occurs at the age of 1.5–2.5 years. As a rule, the first prosthesis is mechanical or pulling. Motorica bionic prostheses are available from 8–11 years old. The age range is quite wide — the possibility of installation is determined by the child’s physical development, height, weight, length of limbs and other factors. All children grow at different rates, and it is important that the smallest size of the bionic arm is not too big for the child.
Thus, the first prostheses are installed in children at the age of six months, and active devices — from 1.5–2 years. If a two-year-old child can handle the task, then an adult of any age clearly can do it as well. Knowing how to use a prosthesis is a skill, just like driving a car or cooking borshch. It may not work right away, but you can achieve success through training. If you have missed all the time frames described above, this does not mean that you would fail to adapt to the device, or that it is already “too late” for prosthetics. Adaptation will require more effort, but it is definitely possible. We have many such examples.
Why is prosthetics recommended at six months? Because at about this age the child begins to sit up, and this is a task that requires a sense of equilibrium. “Catching” this equilibrium requires relatively equal weight of the hands.
Next, the baby masters new motor functions — crawls, stands up, begins to walk — and they also need an even load on both sides of the body. It is important to understand: the more part of the arm is missing, the greater the need for a cosmetic prosthesis from a very early age.
The transition to an active prosthesis occurs at the age of 1.5–2.5 years. As a rule, the first prosthesis is mechanical or pulling. Motorica bionic prostheses are available from 8–11 years old. The age range is quite wide — the possibility of installation is determined by the child’s physical development, height, weight, length of limbs and other factors. All children grow at different rates, and it is important that the smallest size of the bionic arm is not too big for the child.
Thus, the first prostheses are installed in children at the age of six months, and active devices — from 1.5–2 years. If a two-year-old child can handle the task, then an adult of any age clearly can do it as well. Knowing how to use a prosthesis is a skill, just like driving a car or cooking borshch. It may not work right away, but you can achieve success through training. If you have missed all the time frames described above, this does not mean that you would fail to adapt to the device, or that it is already “too late” for prosthetics. Adaptation will require more effort, but it is definitely possible. We have many such examples.
What is important to understand before prosthetics?
Simply putting a prosthesis on the arm is not sufficient — it is important to understand how it works, perform daily exercises, and motivate yourself in difficult moments. The success of prosthetics depends 50% on the prosthetic company and 50% on yourself.

Why can’t one put on a prosthesis right away or why is preparation necessary?
Some people wear a prosthesis every day and are able to thread a needle with the help of the prosthesis, while others use the prosthesis once a week for 15 minutes or put it away on a shelf altogether. Preemptively, we may say that extreme scenarios — for example, you feel embarrassed to go outside without a prosthesis or, on the contrary, do not wear a prosthesis at all — are considered a failure. The most correct scenario is that the individual is adapted to everyday life both with and without a prosthesis. In this scenario, the prosthesis is used regularly (daily) for independently selected activities.
What influences whether a prosthesis will be comfortable to use regularly? There are many factors, and one of them is preparation for prosthetics. In some cases of injuries and amputations, especially in the postoperative and early recovery period, the work of a medical rehabilitation team will be necessary.
What influences whether a prosthesis will be comfortable to use regularly? There are many factors, and one of them is preparation for prosthetics. In some cases of injuries and amputations, especially in the postoperative and early recovery period, the work of a medical rehabilitation team will be necessary.
Who can help prepare for prosthetics?
During preparation for prosthetics, you may (or, sometimes, you should) call on resources of rehabilitation centers, both public and private. These centers can provide a comprehensive health assessment and select exercises to develop those aspects, which are required for prosthetics specifically for you.
At your first meeting with a rehabilitation therapist or a physical therapy doctor, tell them that you are preparing for prosthetics and that therefore you would like to focus on creation of sufficient strength in the arm muscles and sufficient range of motion, expansion and improvement of your existing abilities for self-care and use of the arm in everyday life, development of coordination skills and improvement of the general stamina. We will discuss these goals in more detail below.
A modern rehabilitation team necessarily includes a psychologist and an ergotherapist. A psychologist is able to more thoroughly prepare you for prosthetics, help you “live through” the loss of a limb, understand fears, teach how to respond correctly to uncomfortable questions, and to tell you how to properly motivate yourself to use a prosthesis. When a limb is lost as a result of injury or surgery, working with a psychologist often comes to the forefront. Keep in mind that if you cannot find a suitable specialist in your location, you can consider the possibility of remote sessions. Nowadays, they are quite accessible and effective. A psychologist can work immediately with you or with your family members if needed.
An ergotherapist is a specialist whose work is aimed at maximizing a person’s adaptation to the environment, taking into account preserved functions, and at developing hand motor skills. The user is able to prepare the hand for prosthetics, and later teach how to use the prosthesis, and select special devices to enhance the individual’s capabilities, if necessary. The term “ergotherapist” is new for our country; these specialists are few in number. If you cannot find an ergotherapist, you can try to resort to an occupational therapist/social adaptation specialist, or discuss the above tasks as a part of working with a physical therapy doctor/trainer. Do not hesitate to contact Motorica for the necessary contacts.
At your first meeting with a rehabilitation therapist or a physical therapy doctor, tell them that you are preparing for prosthetics and that therefore you would like to focus on creation of sufficient strength in the arm muscles and sufficient range of motion, expansion and improvement of your existing abilities for self-care and use of the arm in everyday life, development of coordination skills and improvement of the general stamina. We will discuss these goals in more detail below.
A modern rehabilitation team necessarily includes a psychologist and an ergotherapist. A psychologist is able to more thoroughly prepare you for prosthetics, help you “live through” the loss of a limb, understand fears, teach how to respond correctly to uncomfortable questions, and to tell you how to properly motivate yourself to use a prosthesis. When a limb is lost as a result of injury or surgery, working with a psychologist often comes to the forefront. Keep in mind that if you cannot find a suitable specialist in your location, you can consider the possibility of remote sessions. Nowadays, they are quite accessible and effective. A psychologist can work immediately with you or with your family members if needed.
An ergotherapist is a specialist whose work is aimed at maximizing a person’s adaptation to the environment, taking into account preserved functions, and at developing hand motor skills. The user is able to prepare the hand for prosthetics, and later teach how to use the prosthesis, and select special devices to enhance the individual’s capabilities, if necessary. The term “ergotherapist” is new for our country; these specialists are few in number. If you cannot find an ergotherapist, you can try to resort to an occupational therapist/social adaptation specialist, or discuss the above tasks as a part of working with a physical therapy doctor/trainer. Do not hesitate to contact Motorica for the necessary contacts.
Global goals in preparation for prosthetics
Creation of sufficient arm muscle strength.
We try to make our prostheses as light as possible; nevertheless, a prosthesis for an individual’s arm is an additional and unusual weight. In order for the arm to get tired less, move better and for the prosthesis to “obey” better, the muscles need to be prepared for the future load, that is, their strength needs to be trained. In some cases, it is also necessary to work on increasing the range (scope) of motion in the joints. However, we warn about such cases individually and try to select a set of special exercises, or refer for in-person rehabilitation.
We try to make our prostheses as light as possible; nevertheless, a prosthesis for an individual’s arm is an additional and unusual weight. In order for the arm to get tired less, move better and for the prosthesis to “obey” better, the muscles need to be prepared for the future load, that is, their strength needs to be trained. In some cases, it is also necessary to work on increasing the range (scope) of motion in the joints. However, we warn about such cases individually and try to select a set of special exercises, or refer for in-person rehabilitation.
Expansion and improvement of the existing abilities for self-care and use of the hand in everyday life.
Generally, most of our patients with a unilaterally specific limb are fully adapted to everyday life. Zippers and laces are common difficulties, but these are minor problems.
The situations that really worry us are when the individual is completely unable to cope with normal daily living tasks unassisted, i.e. the user is largely dependent on other people in all or many aspects of life. It would be very difficult to encourage yourself to start doing something with the prosthesis, because the hand is simply not used to working. Now is the time to amend the situation, even if it concerns very simple, basic things.
This argument is especially important for people with double amputations or patients with combined diseases (other than diamelia). There are various assistive devices for dressing, cooking, and so on. Feeling independent and being independent is very important.
The situations that really worry us are when the individual is completely unable to cope with normal daily living tasks unassisted, i.e. the user is largely dependent on other people in all or many aspects of life. It would be very difficult to encourage yourself to start doing something with the prosthesis, because the hand is simply not used to working. Now is the time to amend the situation, even if it concerns very simple, basic things.
This argument is especially important for people with double amputations or patients with combined diseases (other than diamelia). There are various assistive devices for dressing, cooking, and so on. Feeling independent and being independent is very important.
Development of coordination skills, which help quickly master the control of a prosthesis.
There are many examples showing that children and adults who have been involved in sports requiring good coordination and then lost a limb, learn to use a prosthesis much faster. They feel much more confident than their peers without sports experience. What does this mean for us? The better an individual feels the body as a whole and the better they can control it, the easier they would be able to adapt to the prosthesis.
Improvement of the posture and correction of its changes.
For good arm movements, the body must be very stable. A strong body is the foundation underlying all our movements.
Improvement of the posture and correction of its changes.
For good arm movements, the body must be very stable. A strong body is the foundation underlying all our movements.

When should you start preparation?
Preparation needs to start today. The more time we have to prepare, the better we can work on all the aspects mentioned above.
In addition, it is known that it takes at least three weeks to develop a lasting habit. Some scientists indicate 66 days. One way or another, if we start early, by the time the prosthesis is installed a useful habit will have been developed, and adding the use of a prosthesis to this habit will be easier.
If our prosthetists and doctors have informed you that it will take some time to collect the documents, this gives you a head start in terms of preparation. Please do not delay starting the work.
In addition, it is known that it takes at least three weeks to develop a lasting habit. Some scientists indicate 66 days. One way or another, if we start early, by the time the prosthesis is installed a useful habit will have been developed, and adding the use of a prosthesis to this habit will be easier.
If our prosthetists and doctors have informed you that it will take some time to collect the documents, this gives you a head start in terms of preparation. Please do not delay starting the work.

General approach to training
We remind you that this tutorial is of a general nature; it is not suitable for patients in the early postoperative period and has no regard to individual health characteristics. As we have already stated above, the adequate option is the in-person work of an interdisciplinary team to prepare for prosthetics. If this is not possible, print out this guide and contact your doctor or traumatologist/orthopedist for an in-person consultation and “admission” to independent training.
If you are admitted to trainings at home
The main rule of independent training at home is to focus on your physical sensations. If you feel muscle pain, tingling in the chest, or numbness while doing the exercise, stop and consult a specialist. A little discomfort is normal, but pain is a contraindication to training.
We do not recommend independent training with additional weights, especially heavy weight (in this case, the technique of performing the exercise does matter; it can be difficult to figure this out on your own). During training at home follow the rule — start with a warm-up, proceed with the main part and cool down at the end.
Remember, it is better to do less but regularly than more but once a week.
We do not recommend independent training with additional weights, especially heavy weight (in this case, the technique of performing the exercise does matter; it can be difficult to figure this out on your own). During training at home follow the rule — start with a warm-up, proceed with the main part and cool down at the end.
Remember, it is better to do less but regularly than more but once a week.
CAUTION! Before performing exercises, consult your doctor and ask if there are any contraindications to certain movements and loads.
See examples of warm-up and cool-down exercises in the article
“Proper warm-up as a part of preparation for prosthetics."
“Proper warm-up as a part of preparation for prosthetics."
